PICC team helps improve patient care and flow
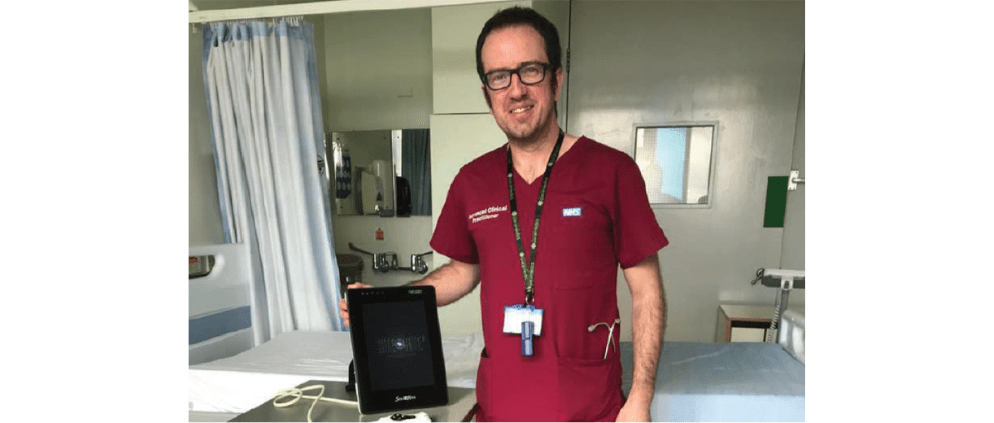
On BD IV News this month, we are pleased to present an interview with Christopher Graham, Advanced Clinical Practitioner – Neurosurgery at the NHS Hull University Teaching Hospitals. In an insightful interview, Mr Graham spoke to us about his centre, and how BD solutions helped improve patient vascular access protocols. He also discussed the benefits that his patients have enjoyed following the implementation of a PICC team, and what are future opportunities for vascular access in his centre.
Can you give our readers a small introduction to your centre?
Hull University Teaching Hospitals Trust is a tertiary neurosurgical centre in the east of Yorkshire, Northern England. It serves a population of about 1.3 million people. The unit itself has approximately 50 beds and is a major trauma centre as well as a neurosurgical unit. It provides the full range of neurosurgical interventions.
More on this topic: PICC line or port catheter: Which one for cancer patients?
What are the challenges you faced that prompted you to review your centre’s vascular access protocols?
The historical practice in neurosurgery for vascular access was peripheral cannulation in the first instance, and then the next option was either a central line or Hickman line. Now, in neurosurgery, we have a lot of critical patients who need longer-term IV access. We had no alternative options to enable patient treatment. On top of that, we also manage a lot of neurosurgical infections, whether it be post-operative or in presentation with conditions such as a brain abscess or a spinal infection. Many of these require several months of IV antibiotics.
So, Hickman lines were placed by the theatre and the vascular teams. This was not a service as such and was very ad hoc. It was done when there was a spare place on the vascular surgeon’s list at the end of the day or on a dedicated list, occasionally on a Wednesday afternoon, which meant long waiting times for longer-term IV access. A lot of our patients were fit for discharge before this and would have been able to go to our outpatient antibiotic department.
However, we were using a lot of bed days in the acute neurosurgical centre with patients purely waiting for IV access. That was the initial driver for being able to place PICCs (peripherally inserted central catheters) ourselves. Additionally, a lot of our sick patients require intensive IV fluid therapy, even regular blood and often TPN (Total Parenteral Nutrition). So, for inpatients being able to achieve reliable longer-term IV access was also a benefit.
How did you go about setting up the PICC team?
The initial process involved identifying the patient groups that we would target. We estimated this to be around about 120 to 150 patients per year. We then wrote a business case with the support of BD. This was because, having looked at the literature on the product, we felt that the BD Site-Rite™ 8 with the BD Sherlock 3CG™ tip confirmation system was something that would facilitate our aim of being able to place the lines easily at the bedside without the need for X-rays.
It also avoided us taking critically unwell patients away from a ward or transferring them to X-ray departments and gave us instant access to the therapies that the patients needed. The business case was a slow process. Finding the funds to set up a new service was challenging. That was when we decided to take a loaned machine which was kindly given by BD. Using this, we could prove our business case.
Can you tell us something about the BD® solutions that you used (BD Site-Rite™ 8 ultrasound and BD PowerPICC Solo™)? What were the factors that led you to choose these?
The package of the BD Site-Rite™ 8 and the BD Sherlock 3CG ™ is perfect for use in combination with the BD PowerPICC Solo™. We are a centre that uses a lot of contrast for our imaging. Therefore, we need power injectable PICC and midline devices.
Were the education and support provided useful for you?
The support was excellent, to be quite honest. Because our service was very much an on-demand service rather than a set-date-and-place, we were required to place lines potentially within 24 hours of identifying the need for one – and that is essentially acute care. The support in terms of that was very good and at short notice. The flexibility to attend and support us in training and placing the lines around our departmental workload was key for us to develop the service and in enabling our practitioners to continue the work.
Can you tell us how the PICC team has improved vascular access in your centre? How have the centre and its patients benefitted?
From many angles, it has improved. We are getting timely, appropriate access to our patients. We are inserting the lines essentially the same day that we recognize the demand for IV access. It has avoided delays in treatment and has improved our flow through the department. Our turnaround for patients is much quicker. When they are ready to go, they have got the appropriate IV access and are out and back home, which is particularly pertinent during the COVID-19 pandemic.
More on this topic: PICC lines: comparing infections in cancer vs noncancer patients
What according to you, are the main takeaway lessons from your centre’s experience with a PICC team?
Identify your patient group, be very specific, be realistic with what you are trying to achieve, and do not take too much on too early. Our service has developed over several years. Initially, we started with PICC lines with a small group of patients which has expanded as we have got used to the equipment and are recognising its potential.
We have extended into conventional midlines and we are now looking into using the BD PowerGlide Pro™ Midline Catheter as well, so we can have a full complement of IV access in the department at our disposal. The main takeaway lessons are to have a strong business case and time.
What does the future of vascular access at your centre look like?
What we are aiming for is having a full complement of options for IV access in-house and ready to use. We will have the full capacity from peripheral cannulation to the BD PowerGlide Pro™ Midline Catheter to PICC lines, which we can essentially tailor to our patient needs. Whether it be a week-long IV therapy or several months, we will be able to efficiently manage our patient numbers and be prepared for future demands.
References
Disclaimer: The views expressed by the interviewee are his personal opinions.
Approval number BD-30545.
![]()
![]()