3 factors to consider in vascular access device selection
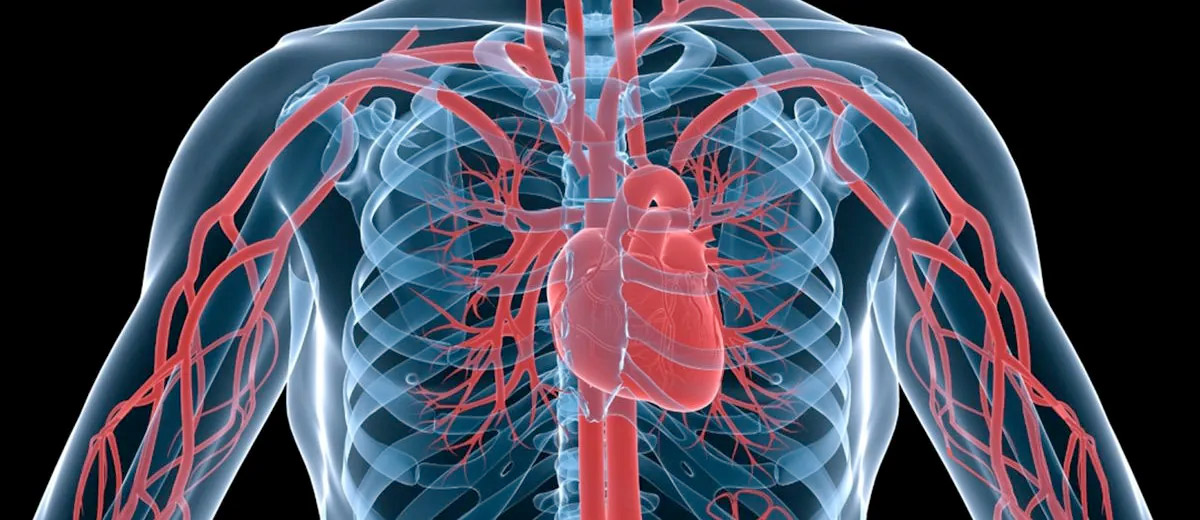
Vascular access device (VAD) selection represents a crucial moment in vascular access management (VAM).
“A peripheral vessel selection is not the same as a central vessel selection because when we look at tips for haemodilution, we can run anything through a central line… [For] peripheral circulation, we have to be very much aware of pH, osmolarity and the vesicant nature of our drug; how we’re administering this drug and for how long…” according to Kathy Kokotis, Director of Market Development, BD.
Ms Kokotis spoke on “How to choose the appropriate VAD for your patients?” on the first day of BD MACOV@23, a virtual edition of the Multidisciplinary Advanced Course on Vascular Access (MACOVA) held on 5–7 September 2023. She highlighted three crucial factors which should be considered when selecting a VAD.
Factor 1: Take the patient’s vasculature into account for vascular access device selection
When assessing a patient’s vascular anatomy, examine vein diameter and blood flow.1
Vein diameter can vary based on changes in temperature:
- Cephalic vein at the wrist: 2.8–3.4 mm2
- Cephalic vein near the cubital fossa: 3.1–3.5 mm2
- Basilic vein near the cubital fossa: 5.1–5.5 mm2
- Superior vena cava: up to 20 mm3
If more than one third of a blood vessel is occupied by a catheter, this may reduce blood flow to the area.4 This increases the risk of VAD-related thrombosis.4 The haemodilution of medication administered intravenously depends on blood volume and flow velocity.5 It is thus important to choose a VAD with the smallest outer diameter.1
More on this topic: How to identify and reduce the risk of catheter-related thrombosis
Factor 2: Consider infusate characteristics for vascular access device selection
Let’s start with pH levels and osmotic concentrations. With regards to pH, infused solutions/medications should be isotonic and euhydric (i.e., physiological pH).6 Excessive pH or osmolality increase the risk for possible damage to veins or blood cells.6
For example, when considering whether to use a central vascular access device (CVAD) or peripheral vascular access device (PVAD) for infusing parenteral nutrition (PN), the eighth edition of the Infusion Therapy Standards of Practice recommends choosing a CVAD for final PN concentrations that generate an osmolarity rate of over 900 mOsm/L.1
According to the World Congress on Vascular Access (WoCoVA), there is broad consensus in the literature on using CVADs for infusions with osmolarity rates of over 600 mOsm/L and pH levels below 5 or above 9.7 Other infusate characteristics to keep in mind when selecting a VAD include verifying if the substance that will be infused is an irritant or vesicant.1
An irritant is, “An agent capable of producing discomfort (e.g., burning, stinging) or pain as a result of irritation in the internal lumen of the vein with or without immediate external signs of vein inflammation.”1 A vesicant is, “An agent capable of causing tissue damage when it escapes from the intended vascular pathway into surrounding tissue.”1
According to the European recommendations on the proper indication and use of peripheral venous access devices (ERPIUP), irritants and vesicants should preferably be administered via a CVAD.7 In addition to the above considerations, it is recommended that each ward have a list of peripherally incompatible intravenous medications.7 This can be helpful when choosing whether to use a PVAD or CVAD.7
More on this topic: PICC line or port catheter: Which one for cancer patients?
Register to read the full article and watch Ms Kokotis’ presentation
References
- Gorski LA, Hadaway L, Hagle ME, et al. Infusion Therapy Standards of Practice, 8th Edition. J Infus Nurs. 2021;44(1S Suppl 1):S1-S224. doi:10.1097/NAN.0000000000000396
- Irfan H, Ooi GS, Kyin MM, Ho P. Revealing Maximal Diameter of Upper Limb Superficial Vein with an Elevated Environmental Temperature. Int J Chronic Dis. 2016;2016:8096473. doi:10.1155/2016/8096473
- White HJ, Soos MP. Anatomy, Thorax, Superior Vena Cava. StatPearls Publishing; 2023.
- Moureau N, ed. Vessel Health and Preservation: The Right Approach for Vascular Access. 1st ed. Springer Cham; 2019.
- Ryder M, Gunther RA, Nishikawa RA, et al. Investigation of the role of infusate properties related to midline catheter failure in an ovine model. Am J Health Syst Pharm. 2020;77(16):1336-1346. doi:10.1093/ajhp/zxaa175
- Roethlisberger D, Mahler HC, Altenburger U, Pappenberger A. If Euhydric and Isotonic Do Not Work, What Are Acceptable pH and Osmolality for Parenteral Drug Dosage Forms? J Pharm Sci. 2017;106(2):446-456. doi:10.1016/j.xphs.2016.09.034
- Pittiruti M, Van Boxtel T, Scoppettuolo G, et al. European recommendations on the proper indication and use of peripheral venous access devices (the ERPIUP consensus): A WoCoVA project. J Vasc Access. 2021;24(1):165-182. doi:10.1177/11297298211023274
- Dychter SS, Gold DA, Carson D, Haller M. Intravenous therapy: a review of complications and economic considerations of peripheral access. J Infus Nurs. 2012;35(2):84-91. doi:10.1097/NAN.0b013e31824237ce
- Magallón-Pedrera I, Pérez-Altozano J, Virizuela Echaburu JA, Beato-Zambrano C, Borrega-García P, de la Torre-Montero JC. ECO-SEOM-SEEO safety recommendations guideline for cancer patients receiving intravenous therapy. Clin Transl Oncol. 2020;22(11):2049-2060. doi:10.1007/s12094-020-02347-1
This list of references to third-party peer-reviewed material and the sites they are hosted on are provided for your reference and convenience only, and do not imply any review or endorsement of the material or any association with their operators. The Third-Party References (and the Web sites to which they link) may contain information that is inaccurate, incomplete, or outdated. Your access and use of the Third Party Sites (and any Web sites to which they link) is solely at your own risk.
This presentation contains the personal and professional opinions of the individual speaker and are not necessarily those of Becton, Dickinson and Company (“BD”) or any Business Unit or affiliate of BD. The speaker has been compensated by BD for the time and effort in preparing the material in this presentation.
BD-107872