Lessons learned from preventing central venous catheter bloodstream infections in the United States can be applied to Europe
Dr William R. Jarvis, President of Jason and Jarvis Associates, LLC
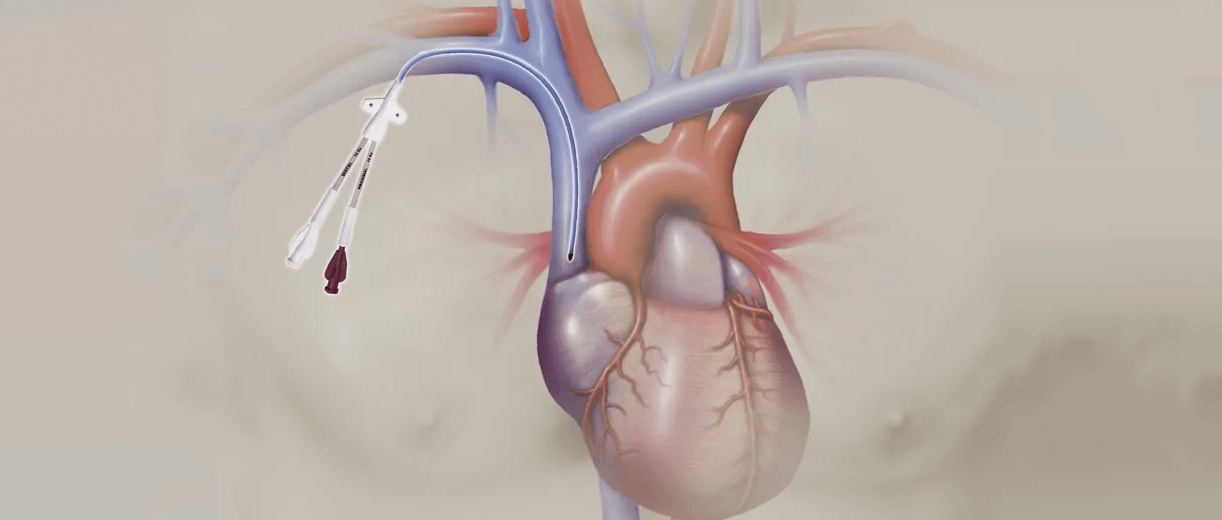
The impact of catheter-related bloodstream infections (CRBSIs) is significant in terms of morbidity and mortality1,2. According to Dr Jarvis, bloodstream infection rates vary by the type of intravenous (IV) catheter used.
Dr Jarvis explained that they also differ from one kind of intensive care unit (ICU) to the next. Each hospital uses a different mix of IV catheters. This makes it difficult to benchmark or compare infection rates between hospitals.
In the first part of “The epidemiology of catheter-related infections (CRIs)” webinar, Dr William R. Jarvis presents statistics showing the incidence of CRBSIs and their clinical impact on patients and economic impact on hospitals and healthcare systems:
626 CRBSIs occurred in the European Economic Area (EEA) in 2011-123
Approximately 40% of all bloodstream infections reported in the EEA in 2011-12 were catheter related3
7 days on average were added to each hospital stay following a CRBSI4
Dr Jarvis then focuses on central venous catheter bloodstream infections (CVC-BSIs).
It is important to keep in mind that risk varies between CVCs1. For example, the highest rates have been reported in non-tunneled centrally-inserted central catheters (CICCs) (12.6 infections per 1,000 line days) while PICCs had a much lower rate (1.81 infections per 1,000 line days)1.
CVC-BSI risks and how to mitigate them
He then goes on to identify several risk factors:
- Length of catheterisation or dwell time
- Insertion site
- Number of catheter lumens
- Maximal barrier precautions (MBPs)
- Skin antiseptics
- Total parenteral nutrition
- Makeup of nursing staff and workload
- Catheter-related thrombosis
But these different risk factors can be managed through prevention recommendations given by Dr Jarvis throughout his talk. He suggests keeping the considerable cost of CVC-BSIs in mind when investing in interventions to prevent them.
Renowned infection prevention expert
Dr Jarvis is currently president of Jason and Jarvis Associates, LLC. He has over 40 years of experience working on healthcare epidemiology and healthcare-associated infection prevention. As a director at the U.S. Centers for Disease Control and Prevention (CDC) for more than two decades, he led over 150 outbreak investigations in the United States and around the world.
Webinar series for vascular access professionals
His talk is part of the MEDical EXperts (MEDEX) webinar series brought to you by BD. MEDEX will be your ongoing source of information, about day-to-day clinical practices, pertaining to infection prevention and control for patients with vascular access devices, medication safety, occupational hazards, evidence-based best practices, standards and recommendations from experts.
The BD IV News team will present other MEDEX webinars in future articles. Find out how you can prevent CVC-BSIs in your healthcare organisation by clicking on the link below.
#vascularaccess #bloodstreaminfection #catheterrelatedinfection #centralvenouscatheter #healthcareassociatedinfection #infectionprevention #ivtherapy #patientsafety
References
This list of references to third party peer reviewed material and the sites they are hosted on are provided for your reference and convenience only, and do not imply any review or endorsement of the material or any association with their operators. The Third Party References (and the Web sites to which they link) may contain information that is inaccurate, incomplete, or outdated. Your access and use of the Third Party Sites (and any Web sites to which they link) is solely at your own risk.
1. Mollee P, Jones M, Stackelroth J, et al. Catheter-associated bloodstream infection incidence and risk factors in adults with cancer: a prospective cohort study. J Hosp Infect. 2011;78(1):26-30. doi: 10.1016/j.jhin.2011.01.018.
2. Wang EW, Layon AJ. Chlorhexidine gluconate use to prevent hospital acquired infections-a useful tool, not a panacea. Ann Transl Med. 2017;5(1):14. doi: 10.21037/atm.2017.01.01.
3. European Centre for Disease Prevention and Control (ECDC). Surveillance report. Point prevalence survey of healthcare associated infections and antimicrobial use in European acute care hospitals 2011–2012. Stockholm: European Centre for Disease Prevention and Control (ECDC); 2013.
4. Bicudo D, Batista R, Furtado GH, Sola A, Medeiros EA. Risk factors for catheter-related bloodstream infection: a prospective multicenter study in Brazilian intensive care units. Braz J Infect Dis. 2011;15(4):328-331. Published 2011/08/24.
This presentation was developed by the presenter, and the findings, interpretations, and conclusions contained or expressed with it do not necessarily reflect the views of BD. To the extent this presentation relates to specific products, such products should always be used in accordance with the relevant instructions for use and other product documentation. This content should not be copied or distributed without the consent of the copyright holder. For further information, please contact: GMB-EU-MDS@bd.com
Approbation number: BD-21892