Finding the right fit to prevent misconnection errors
BD sponsored a symposium on “Safe connections in regional anaesthesia.” It was held at the 3rd European Society of Regional Anaesthesia & Pain Therapy (ESRA) international e-congress on Saturday, 19 September 2020. A representative of BD began the symposium by introducing Professor Dan Benhamou. He then presented the results of a systematic literature review.
A Literature Review: Data to support the frequency & impact of misconnections
Stephen Church, Director Medical Affairs, BD Medication Delivery Solutions
Searches were performed of English-language publications or abstracts published over a 20-year period (1 January 1999- 30 September 2019) on PubMed, Embase and the Internet1.
Inclusion and exclusion criteria
Inclusion criteria were: case reports and studies with confirmed wrong-route errors and misconnection events1. These had to mention the name of the drug administered as well as patient outcomes following each event1.
The authors excluded cases involving wrong-route errors that were not related to misconnection1. Out of approximately 200 articles, 72 were included in the systematic literature review (publication forthcoming)1.
Misconnection-related errors
Out of 130 misconnection errors identified, the most common involved epidural medication administered intravenously, or intravenous (IV) medication administered via the epidural route1.
The following risk factors were identified for misconnection-related incidents2:
- Luer connector’s ease-of-use
- Workarounds
- “Automatic” mode because of stress, fatigue or distractions
- Poor lighting and other environmental factors
- Placing dissimilar tubing next to each other
- Not checking connections after patient transitions
- Suboptimal reporting of adverse events and near misses
Patient outcomes
There was a significant number of deaths (24) and severe events (8) that resulted from these errors1. He also presented data from different European countries showing numbers of wrong-route errors over different periods of time1.
In conclusion, the ubiquitous nature of the luer connector presents a risk to patients1. The number of misconnection errors is relatively low1. However, they can be severe and possibly lead to death1. These errors can be prevented.
ISO 80369-6 (NRFit™): What is it, how did it evolve and what are the implications for regional anaesthesia?
Professor Dan Benhamou, Department of Anesthesia Resuscitation Perioperative Medicine, Assistance Publique – Hôpitaux de Paris (AP-HP), Université Paris Saclay, Hôpital Bicêtre, France
Sounding the alert
In March 2007, the U.K. National Patient Safety Agency (NPSA) of the National Health Service released a patient safety alert on “Safer practice with epidural injections and infusions3.” This document made several recommendations designed to reduce the risk of epidural administration errors3.
An alert released in 2009 from the NPSA stated, “All spinal (intrathecal) bolus doses and lumbar puncture samples are performed using syringes, needles and other devices with safer connectors that will not connect with intravenous Luer connectors4.”
Alternatives to Luer connectors
The NPSA gave the medtech industry and healthcare until 1 April 2013 to conform to these new guidelines4. Several manufacturers created alternatives to Luer connectors, but these did not prevent misconnection errors entirely3.
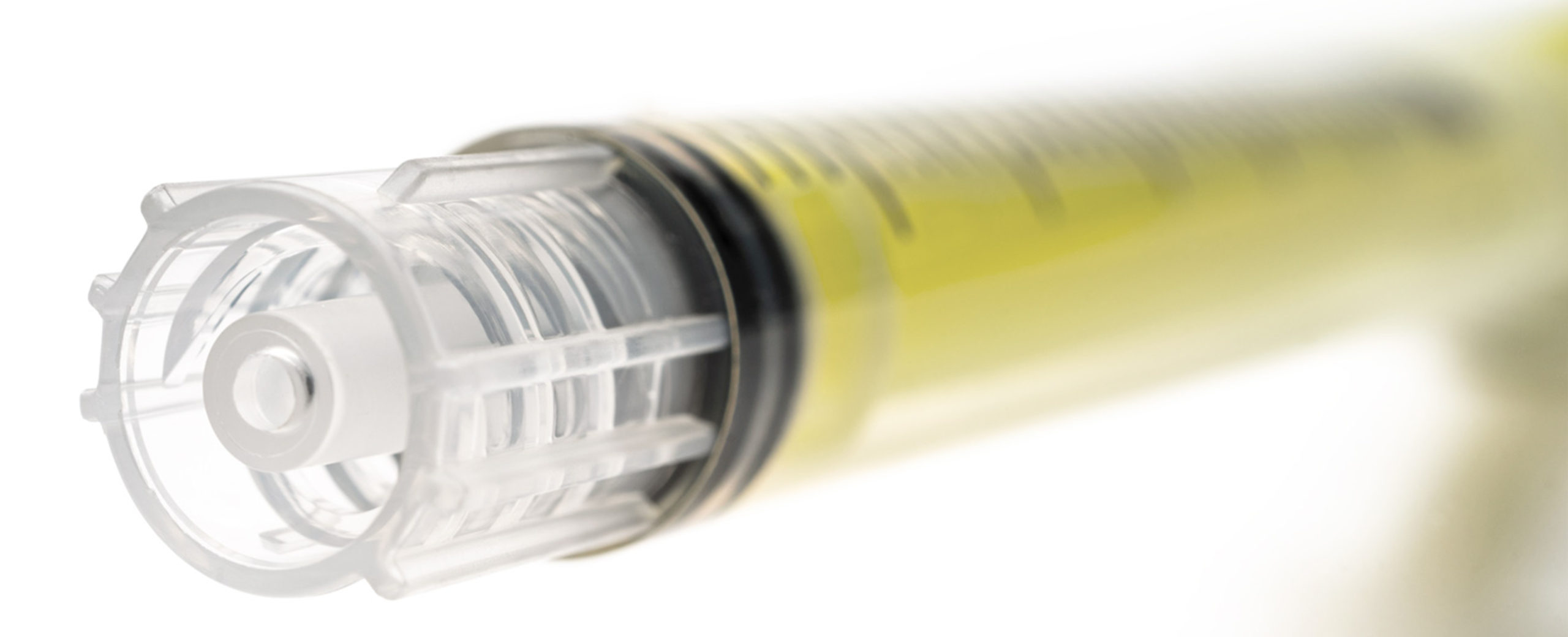
International Standardisation Organization (ISO) 80369 group of standards was created to address the problem3. ISO 80369-6, the connector developed for regional anaesthesia, was launched in 20173. The Global Enteral Device Supplier Association (GEDSA), a group of medical device manufacturers decided to call it NRFit™ for neuraxial fit3.
He concluded by saying challenges remain and recommended careful planning during the transition to NRFit™ connectors3. He also emphasised the fact that misconnection error prevention requires several solutions, but this forcing function is an effective way of protecting patients from harm3.
#errorprevention #iso80369 #medicationerror #nrfit #patientsafety #regionalanaesthesia #spinalanaesthesia
References
1. Church S. A Literature Review: Data to support the frequency & impact of misconnections. Presented at: 3rd European Society of Regional Anaesthesia & Pain Therapy (ESRA) international e-congress; 2020.
2. Patient Safety Advisory Group. Managing risk during transition to new ISO tubing connector standards. Sentinel Event Alert 2014; (53): 1-6.
3. Benhamou D. ISO 80369-6 (NRFit™): What is it, how did it evolve and what are the implications for regional anaesthesia? Presented at: 3rd European Society of Regional Anaesthesia & Pain Therapy (ESRA) international e-congress; 2020.
4. National Patient Safety Agency (NPSA). Patient Safety Alerts NPSA/2009/PSA004A and NPSA/2009/PSA004B: Safer spinal (intrathecal), epidural and regional devices – Part A and Part B. London, United Kingdom: U.K. National Health Service; 2009.
This list of references to third party peer reviewed material and the sites they are hosted on are provided for your reference and convenience only, and do not imply any review or endorsement of the material or any association with their operators. The Third Party References (and the Web sites to which they link) may contain information that is inaccurate, incomplete, or outdated. Your access and use of the Third Party Sites (and any Web sites to which they link) is solely at your own risk.
This presentation was developed by the presenter, and the findings, interpretations, and conclusions contained or expressed within it do not necessarily reflect the views of BD. To the extent this presentation relates to specific products, such products should always be used in accordance with the relevant instructions for use and other product documentation. This content should not be copied or distributed without the consent of the copyright holder. For further information, please contact: GMB-EU-MDS@bd.com